Under the risk adjustment (RA) model, reimbursements to the insurance companies (Plans) are based on the member’s level of severity of illness rather than the number and types of interventions the member receives throughout the year. This reimbursement model is based on documentation by the provider of their patient’s chronic and acute conditions and the associated diagnosis codes. Risk adjustment is used by the Center for Medicare and Medicaid Services (CMS) as well as the U.S. Department of Health and Human Services (HHS) for patients covered under Medicare, Medicaid and commercial programs as well as specialty programs such as the Programs of All-Inclusive Care for the Elderly (PACE), End-Stage Renal Disease (ESRD) and for Dual-eligible Special Needs Plans (DSNP). Many of the programs also have a special RA process used for reimbursement to the pharmacy programs.
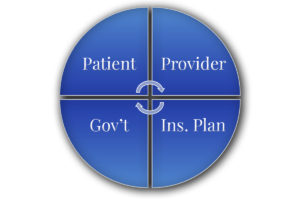
There are four main players in the RA process, and each has a distinct and important role in that partnership that makes the risk adjustment process work. These players are the patient, provider, insurance plan, and responsible government entity.
The Patient
The patient’s role in the partnership is based on their engagement and involvement. A more involved patient seeks care not only when ill but also for routine and preventative visits. Patient involvement can be gauged based on their compliance with medical care and recommendations, being knowledgeable about and aware of their conditions, and demonstrating a willingness to undergo a health risk assessment (HRA) when necessary.
The Provider
The provider is a main partner in the risk adjustment model of care. The provider is responsible for medically-sound decision making for diagnoses and interventions. One important aspect of the provider’s role is their documentation. Diagnosis codes can only be captured from the documentation.
A provider may possess extensive knowledge and make great decisions. However, if they lack the ability to effectively document their thoughts in the patient’s chart, then others are unable to accurately report the provider’s knowledge and actions. Moreover, plans and government entities are focused on rooting out fraud and abuse in the diagnosis submission process. Cases have been brought against those coding diagnosis that are not in the medical record and against those that are documenting in the medical record diagnosis that the patient does not actually have.
Some questions to consider pertaining to the provider’s role in the RA process:
- Does the provider correctly diagnose conditions and document them accurately in the record? If the provider employs medical coders, is there an internal process for compliant queries to communicate between the coder and the provider when questions arise?
- Does the provider organization appropriately maximize the use of EMR functionality including templates, prompts, edits and other timesaving drivers of consistent documentation – without encouraging repetitive copy and paste?
- Is the provider aware of the risk adjustment process and the need for thorough documentation?
- How knowledgeable of coding rules and requirements is the provider if they are involved in coding their own records?
- Is the provider employed directly by the insurer or are they independent? In either case, is their compensation impacted directly or indirectly by plan payments adjusted based on the patient risk score? If yes, are there appropriate controls, quality assurance checks, and other mechanisms of an effective compliance program in place to monitor the accuracy of diagnostic submission. (See my article about updates to the 2024 risk adjustment model and areas to consider for improved clinical documentation1.)
The Plan
The Plan (or insurance company) is the intermediary between the provider and the government. The diagnoses that get reported to the government are submitted by the Plans, and not directly from the providers. The Plan is responsible for reporting the diagnoses to the governmental entity. The Plan is also responsible for reimbursing the providers. Some questions to consider pertaining to the Plan’s role in the RA process:
- Does the Plan use only claims data for reporting or do they also perform direct chart reviews?
- If the Plan performs chart reviews, do they use a retrospective process whereby they review records after the fact, or do they use a concurrent process where they review the records shortly after creation and have a query process for communication between the coding team and the provider for questions?
- Does the Plan have an internal process to ensure all queries between the coder and the provider are compliant, are not leading, and are not solely focused on increasing reimbursement?2
- Does the Plan use a prospective approach whereby they identify potential gaps in care by comparing diagnoses reported in previous periods against what is reported in the current reporting period?
- If a gap is suspected, communication can occur between the Plan and the provider for the opportunity to achieve thorough and accurate documentation of conditions to their highest level of specificity. What is that process? Is the provider able to either agree or disagree with the additional diagnoses?
- Does the Plan have a team of employed providers whose focus is patient evaluation and documentation for risk adjustment purposes only?
- What does the Plan do with the data generated by the RA diagnoses – is there care management for “high-risk” patients? How are they using the data they receive during this process to help better manage their members? Are they focusing on how to improve the partnership with the providers and the patients?
- What is their education plan to their coding staff as well as to the providers regarding the RA program, its rules, requirements, etc.?
The Government
The last partner in this structure is the governmental entity responsible to ensure coverage of its eligible members and provide reimbursement to the insurance company covering the individuals. This entity determines which diagnosis codes are considered “eligible for reimbursement” under the RA program. Additionally, it determines how to convert the diagnosis codes into an actionable number for reimbursement purposes (called the Risk Adjustment Factor or RAF score) and sets the reimbursement amounts and rules. This entity is also responsible to monitor the Plans and ensure the RA program is being implemented correctly and reimbursements are accurate.
Partnership Collaboration
Each partner has their own important role in the risk adjustment process. The patient’s active participation and commitment to seeking and following through with their care is vital. Simultaneously, the provider’s responsibility lies in delivering medically-sound interventions and ensuring comprehensive documentation of all relevant conditions for effective medical management. The Plan, for its part, must reimburse the providers or patients for the care provided while also collecting and validating encounter data before submission to the government entity. Lastly, the government entity assumes the responsibility of developing and monitoring the process, establishing fair rules and reimbursement guidelines, and enforcing them equitably.
Patients, CMS, Medicaid agencies, providers, and Plans all have a role in diagnosis capture. However, the interactions with patients and capture of all relevant clinical information should be separate from the risk adjustment data collection process. When providers make sound medical decisions and document them accurately, the patient’s chart becomes a true and reliable reflection of their medical journey, irrespective of whether they fall under the Risk Adjustment reimbursement model. This documentation serves multiple purposes, including reimbursement, identifying areas for further study, securing funding and support, and monitoring public health concerns by entities like the Centers for Disease Control (CDC). The actual payment process should only come into consideration after all the patient care and clinical documentation is performed resulting in appropriate compensation to those caring for sicker patients.
Reach out to our coding and risk adjustment team members in the Healthcare Compliance practice at SunHawk Consulting, LLC’s if you want to learn more about the intricacies of risk adjustment.

Lorraine Aniello
Clinical Coding Audit Director
SunHawk Consulting, LLC
[email protected]
Lorraine is a Registered Nurse and holds certification as a Certified Professional Coder (CPC), Certified Risk Adjustment Coder (CRC) from the American Academy of Professional Coders (AAPC), and Advanced HCC Auditor (AHCCA) from Rise Health. She is also certified as a HealthCare Anti-Fraud Associate (HCAFA).
Lorraine has been a coding trainer and reviewer for one of the largest U.S. healthcare organizations. Within regulatory organizations, she has worked with state Medicaid policy and program integrity, MFCUs, RACs, MEDIC, and was a corporate clinical trainer for a national vendor who assisted Medicare and Medicaid Advantage companies with risk adjustment data collection, coding and reporting. She has provided testimony and expert analysis for both government prosecutors, litigation counsel, and defense counsel.

James Rose
Managing Director
SunHawk Consulting, LLC
J[email protected]
James Rose is Managing Director of SunHawk Consulting LLC. James is a CPA and also holds certifications in Internal Auditing (CIA), Risk Management Assurance (CRMA), and Information Systems Auditing (CISA, CISSP). James is an experienced healthcare operations, governance, risk, and compliance executive focused on the healthcare and governmental industries. Most recently he served as Chief Financial Officer of Aperture Credentialing LLC, where he was also accountable for many of the traditional Chief Operating Officer duties in addition to CFO / Controller responsibilities. He currently serves as an expert advisor to the World Health Organization’s Staff Health Insurance Global Oversight Committee (providing his expertise on health and wellness programs as well as medical insurance cost management and financial planning). James is also Chair of the Jefferson County Public Schools Audit and Risk Advisory Committee.

Rachael Mills
Managing Consultant
SunHawk Consulting, LLC
[email protected]
Rachael Mills is a Managing Consultant with SunHawk Consulting, LLC and is experienced in medical claims analytics, statistical analysis, compliance assessments, GRC (governance, risk and compliance) platform configuration and overall project and program management. She is skilled in compliance program communication development including digital design, brand management, training development, and marketing communications. At a national healthcare credentialing organization Ms. Mills assisted with the design and implementation of both internal and external forms of marketing communications and collateral. At SunHawk, she has supported numerous compliance reviews, HIPAA assessments, statistical engagements, investigations, and GRC tool implementations. Ms. Mills has assisted with annual compliance risk assessments conducted for clients as part of their Corporate Integrity Agreement (CIA) with the Office of Inspector General (OIG), as well as supported SunHawk during Independent Review Organization (IRO) engagements.
See Also:
Aniello, Lorraine. “Are You Ready for the 2024 Risk Adjustment Model?” Edited by James Rose and Rachael Mills, SunHawk Consulting, 2 May 2023, https://sunhawkconsulting.com/2023/05/the-cms-hcc-2024-risk-adjustment-model/
“Guidelines for Achieving a Compliant Query Practice – 2022 Update.” ACDIS, 14 Dec. 2022, https://acdis.org/resources/guidelines-achieving-compliant-query-practice%E2%80%942022-update.
SunHawk experts are highly experienced professionals ready to assist you within our focus areas of:
Healthcare Compliance | Corporate Investigations
Corporate Compliance | Litigation Disputes
Have a question? We are ready to answer it.
